Introduction
Hello, and welcome to English Plus. I’m your host, and this week, we’re embarking on a journey together. A journey not to a distant land, but into the most intricate, awe-inspiring, and sometimes bewildering landscape known to humanity: the three-pound universe nestled between our ears. Our theme and expedition this week is into the vast and often misunderstood territory of brain disorders.
Before we pull back the curtain and begin our deep dive, I want you to take a moment with me. Think about the last time you heard someone say, “It’s all in your head.” Perhaps it was said with a dismissive wave of the hand. Or maybe you’ve said it to yourself, wrestling with a profound sadness that seemed to have no external cause, or a spike of anxiety that felt both overwhelming and illogical. What if that phrase, “it’s all in your head,” wasn’t an invalidation, but a statement of biological fact? What if the head, and the astonishing organ it protects, is precisely the point?
This week, we are asking the big questions, the ones that whisper in the quiet corners of our minds. What truly happens when the organ of our consciousness—the very thing that generates our thoughts, our loves, our fears—experiences a disruption? What is the substantive difference, if any, between a seizure that convulses the body and a depressive episode that paralyzes the will? Why does our society extend a casserole and a sympathy card for a broken leg, but often offers silence and stigma for a condition like bipolar disorder or schizophrenia?
We’re going to confront these questions head-on. We’ll be exploring the delicate and powerful machinery of the brain and asking:
- What exactly is a brain disorder? Is it a glitch in our wiring? A chemical imbalance? A consequence of our environment? Or a complex tapestry woven from all three?
- Why have we constructed such a formidable wall between “neurological” conditions like Parkinson’s or Multiple Sclerosis, and “mental health” conditions like anxiety or PTSD? Are these two separate kingdoms, or are they merely different neighborhoods in the same sprawling, interconnected city of the brain?
- How can understanding the biology of the brain—the simple, revolutionary idea that it is an organ just like our heart or our lungs—completely reframe our perception of these conditions and, in doing so, begin to dismantle the centuries-old stigma that surrounds them?
This is not about providing easy answers or quick fixes. The world of brain health is far too nuanced for that. Instead, this is an invitation. An invitation to cultivate curiosity over judgment, to seek understanding over assumption. This is a primer, a foundational course designed to equip you with a new lens through which to view the human experience. True mastery of any subject, especially one as profound as this, doesn’t come from a single podcast episode; it is born from a commitment to deeper reading, rigorous research, and a sustained, open-minded inquiry. Consider this your starting point, your gateway to a more informed and empathetic perspective.
So, get comfortable. Open your mind. This week, we’re not just talking about disorders; we’re talking about humanity. We’re talking about the very essence of who we are. This is Mind Matters: An Introduction to Understanding Brain Disorders. Let’s begin.
Mind Matters: An Introduction to Understanding Brain Disorders
Hello again, and welcome officially to the first episode of our special theme week, Mind Matters. I’m your host, and I am genuinely thrilled you’ve chosen to join me. We have an ambitious goal this week: to journey together into the heart of what it means to have a brain, and what it means when that brain, for a myriad of reasons, functions in a way that causes distress or dysfunction. Today, we lay the groundwork. We’re drawing the map, defining our terms, and setting our intention for the path ahead. This is our foundational episode, our “Episode Zero,” if you will, for understanding the vast universe of brain disorders.
Our primary task today is to build a container, a broad and inclusive umbrella under which we can gather a whole host of human experiences. The term we’re using for that umbrella is “brain disorder.” Now, that might sound a little clinical, a little stark, but I want to propose that it’s actually the most honest and compassionate term we can use. Because at its core, a brain disorder is any condition that stems from a disruption in the structure or function of the brain, leading to changes in how a person thinks, feels, behaves, or moves.
This definition is intentionally expansive. It’s a big tent. Underneath it, you’ll find conditions that we typically label as neurological. These are the disorders often associated with the brain’s “hardware”—its physical structure, its electrical signaling pathways. Think of epilepsy, with its storms of electrical activity; Multiple Sclerosis, where the protective coating of nerves is damaged; Parkinson’s disease, affecting movement and motor control; or the aftermath of a traumatic brain injury or a stroke. These are conditions that, for the most part, we can see on a brain scan or diagnose with a neurological exam. We view them, correctly, as medical conditions.
But our umbrella also covers what society has historically cordoned off into a separate, often more stigmatized category: mental health conditions, or psychiatric disorders. Here we find depression, which blankets life in a fog of apathy and sadness; anxiety disorders, which put the body’s alarm system on a hair trigger; schizophrenia, which can profoundly alter a person’s perception of reality; Bipolar Disorder, with its dramatic oscillations between emotional poles; or Post-Traumatic Stress Disorder, where a past trauma continues to reverberate in the present.
For centuries, we’ve treated these two categories as fundamentally different. One was a matter of medicine, the other a matter of… what, exactly? A weakness of character? A moral failing? A spiritual sickness? The language we used betrayed our bias. Neurological problems were something you had. Mental health problems were something you were.
The central argument of this entire week, starting right now, is that this distinction is a false dichotomy. It is an outdated, unscientific, and deeply harmful way of thinking. Both neurological and mental health conditions are brain disorders. They both originate in the biology and function of the brain. They are two sides of the same intricate coin. And embracing this unified view is the first, most crucial step toward breaking down the stigma that has caused so much unnecessary suffering for millions.
To truly grasp this, we have to start with the most basic, yet most revolutionary, idea of all.
Part 1: The Brain as an Organ
I want you to perform a little thought experiment with me. Imagine your friend calls you and says, “I have to cancel our dinner plans. My pancreas is acting up again, and my insulin levels are all over the place.” What’s your likely reaction? You’d probably feel a surge of sympathy. You’d say, “Oh no, I’m so sorry to hear that! Is there anything I can do? Please take care of yourself.” You wouldn’t for a moment think, “Wow, what a weak-willed pancreas. If my friend just tried a little harder, they could probably produce the right amount of insulin.” That sounds utterly absurd, doesn’t it?
Now, imagine that same friend calls and says, “I have to cancel. I’m in the middle of a really bad depressive episode and I can’t bring myself to get out of bed.” What’s the reaction now? For many of us, I hope it’s the same empathy. But for many in our society, the internal monologue is… different. It’s laced with judgment. “They just need to snap out of it. They should try to be more positive. Maybe some fresh air would do them good.” We would never tell a person with diabetes to “just snap out of it,” yet we apply this impossibly cruel standard to people whose brains are ill.
This difference in reaction reveals a profound cognitive dissonance in how we view our bodies. We accept, without question, that the heart is an organ that can suffer from heart disease. The lungs can have asthma. The kidneys can fail. The liver can get cirrhosis. These are all biological realities. Yet, we have historically struggled to extend this same basic, biological courtesy to the single most complex organ in the known universe: the human brain.
The brain is not some mystical, ethereal entity that floats above the gritty reality of our physical selves. It is a physical organ. It is three pounds of tissue, fat, and water, composed of an estimated 86 billion neurons, each forming thousands of connections, creating a network of staggering complexity. It runs on electricity and chemicals. It requires oxygen and glucose to function. It has intricate structures with specialized jobs—the amygdala processing fear, the hippocampus managing memory, the frontal lobe orchestrating our executive functions.
And just like any other organ, it can be vulnerable.
It can be damaged by physical trauma, like in a concussion. It can be attacked by the body’s own immune system, as in Multiple Sclerosis. Its intricate chemical signaling systems can become dysregulated. The levels of neurotransmitters like serotonin, dopamine, and norepinephrine—the very molecules that help shape our mood, motivation, and focus—can fall out of their delicate balance. The very structure of the brain can change in response to chronic stress or trauma, forging new neural pathways that reinforce states of fear or hopelessness. The process of apoptosis, or programmed cell death, can go awry. Electrical signals can misfire and cascade into a seizure.
When you look at it this way, the idea of a “brain disorder” becomes much less frightening and mysterious. It becomes a matter of physiology. A person with clinical depression isn’t suffering from a character flaw; they are suffering from a dysregulation in the organ responsible for regulating mood. An individual experiencing a panic attack isn’t being “dramatic”; their amygdala, the brain’s threat-detection center, is malfunctioning and screaming “danger” when there is none. Someone with schizophrenia who hears voices isn’t “making it up”; their auditory cortex is genuinely activating, creating a perception as real to them as the sound of my voice is to you right now.
Seeing the brain as a biological organ is the bedrock of empathy. It shifts the conversation from blame to biology, from shame to science. It allows us to see that these conditions are not choices. They are illnesses. And like all illnesses, they deserve to be met with compassion, care, and a relentless pursuit of effective treatment.
Part 2: The Illusory Divide: Neurological vs. Mental Health
So, if we accept that the brain is an organ and can get sick, why do we still cling so tightly to this division between “neurological” and “mental”? Part of it is history, which we’ll delve into in a later episode. For centuries, anything related to thoughts and emotions was the domain of philosophy and religion, not medicine. The mind was seen as separate from the body—a concept championed by philosophers like René Descartes, who proposed a “mind-body dualism.” This idea has cast a very long shadow.
The traditional, simplistic model often goes something like this: Neurological disorders are “hardware” problems. There’s something physically wrong with the brain tissue, the wiring, the structure. You can often point to it on an MRI. Mental health disorders, in this outdated view, are “software” problems. The hardware is presumed to be intact, but the programming, the code of thoughts and emotions, is buggy.
This hardware/software analogy is, at first glance, appealingly simple. But the more we learn about the brain, the more that analogy completely falls apart. In reality, the hardware and software are so deeply intertwined, so symbiotically linked, that you cannot affect one without profoundly altering the other. They are not separate systems; they are different levels of description for the same integrated system.
Let’s look at the evidence. We now know that chronic depression—a classic “software” problem—can physically shrink the hippocampus, a key brain region for memory and emotional regulation. That is a tangible, measurable “hardware” change. We know that psychotherapy, or “talk therapy”—which seems like a purely “software” intervention—can create new neural pathways and change the way different brain regions communicate with each other. It physically rewires the “hardware.”
Conversely, let’s look at a “hardware” problem. A stroke is a purely neurological event. A blood vessel in the brain is blocked or bursts, causing brain cells to die. It’s a clear-cut hardware failure. And yet, what is one of the most common consequences of a stroke? Depression. Up to a third of stroke survivors experience profound depression. Is that depression a neurological symptom or a mental health condition? The answer is: yes. It’s both. The physical damage to the brain tissue disrupts the chemical and electrical systems that regulate mood.
Consider Parkinson’s disease. We define it by its motor symptoms—the tremors, the rigidity. It’s a classic neurological disorder caused by the death of dopamine-producing cells in a part of the brain called the substantia nigra. It’s a hardware problem. But what do many people with Parkinson’s also experience? Anxiety, depression, and sometimes even psychosis. These are not just psychological reactions to having a difficult illness; they are direct results of the same underlying brain changes that cause the tremors. The depletion of dopamine doesn’t just affect motor control; it affects motivation, reward, and emotional stability.
The line is not just blurry; for all practical purposes, it doesn’t exist. Every single thought you have, every emotion you feel, is the result of a physical process—a cascade of neurotransmitters, a spark of electricity across a synapse. Therefore, a disorder of thought or emotion is, by definition, a disorder of that physical process.
This is why we’re advocating for a unified view of “brain health.” This term elegantly sidesteps the artificial divide. It acknowledges that the brain is a single, integrated organ and that its health is paramount to our overall well-being. Whether a condition manifests primarily as a tremor, a mood swing, a delusion, or a memory lapse, its origin story begins in the brain. Brain health encompasses it all. It’s about ensuring our neural hardware and our experiential software are functioning in harmony. Thinking in terms of “brain health” rather than “mental health versus neurological health” is more accurate, more holistic, and infinitely more productive. It unites patients, researchers, and clinicians under one common cause: understanding and caring for the human brain.
Part 3: The Goals of the Week: Knowledge and Empathy
So, with this foundation laid, what are we trying to accomplish this week? Why are we dedicating an entire series to this topic? We have two explicit, intertwined goals.
Our first goal is to foster understanding through knowledge. Stigma, at its root, is a fear of the unknown. We ostracize what we don’t understand. For centuries, the workings of the brain were a black box, and so the conditions that arose from it were shrouded in superstition, fear, and mythology. People weren’t “depressed”; they were “melancholic” or, worse, possessed. They weren’t experiencing psychosis; they were being punished for their sins.
Science is the most powerful antidote to superstition. By shining a light into that black box—by learning about neurons and neurotransmitters, brain regions and neural networks—we demystify brain disorders. We transform them from terrifying specters into comprehensible, treatable medical conditions. Knowledge empowers us. It gives us the vocabulary to talk about these experiences accurately. It provides a framework for making sense of what can feel senseless. It replaces fear with curiosity. Throughout this week, our aim is to provide you with clear, accessible, and scientifically grounded information that builds a solid foundation of understanding.
But knowledge alone is not enough. And that brings us to our second, and arguably more important, goal: to dismantle stigma through empathy and correct language.
Empathy is the ability to understand and share the feelings of another. It’s what connects us as human beings. But stigma actively destroys empathy. It creates an “us” and a “them.” It judges rather than seeks to understand. Stigma is the invisible barrier that stops someone from seeking help for fear of being seen as “crazy.” It’s the quiet prejudice that makes it harder for someone with a diagnosed mental health condition to get a job or find housing. It’s the subtle but devastating shift in how we treat someone once we learn they have schizophrenia or bipolar disorder.
How do we fight this? We start with ourselves. We start by recognizing the shared biology that underpins all our experiences. We start by listening to the stories of those with lived experience, which we’ll be doing in our next episode. And crucially, we change the way we talk.
Language is not neutral. The words we choose shape our reality and reflect our deepest assumptions. Think about the casual, pejorative way we use clinical terms in everyday life. We say, “The weather is so bipolar today,” or “I’m so OCD about cleaning my kitchen,” or “My ex is a total psycho.”
When we do this, we are not just being imprecise; we are being harmful. We are taking the name of a real, often debilitating illness and reducing it to a caricature, a punchline, an insult. We are trivializing the profound suffering of people who live with these conditions every single day. We are reinforcing the very stigma we claim to oppose.
Throughout this week, we will challenge ourselves to be more mindful, more precise, and more compassionate in our language. We will learn why it’s better to say “a person with schizophrenia” rather than “a schizophrenic,” a small grammatical shift that puts the person first and the diagnosis second. We will explore how we can talk about these topics in a way that is open, honest, and respectful.
Because when we combine knowledge with empathy, something magical happens. We build bridges of understanding. We create safe spaces for vulnerability. We empower people to seek the help they need and deserve without fear of judgment. We begin to heal not just the individual, but the community.
Part 4: A Roadmap for the Week Ahead
So, today was about laying the foundation. We’ve defined our terms, challenged the false divide between the neurological and the mental, and established our mission. But this is just the beginning. To give you a sense of where we’re going, here’s a quick preview of the rest of our Mind Matters week.
Tomorrow, we move from the conceptual to the personal in an episode we’re calling Edustory: The Lived Experience. We’ll be sharing a powerful, anonymized story from someone with lived experience of a brain disorder. It’s one thing to talk about these conditions in the abstract; it’s another thing entirely to hear what it actually feels like from the inside. This episode is all about building that bridge of empathy.
Next, in Types and Categories: Mapping the Mind’s Terrain, we’ll zoom out and look at the major categories of brain disorders. We’ll briefly touch on mood disorders, anxiety disorders, psychotic disorders, neurodevelopmental disorders, and neurodegenerative disorders. The goal isn’t to make you an expert diagnostician, but to give you a basic map of this complex territory, so you understand the key distinctions and commonalities between different conditions.
Following that, we’ll have a whole episode dedicated to a topic we’ve already touched upon today: The Power of Words: A Guide to Responsible Language. We will do a deep dive into the impact of our vocabulary. We’ll discuss stigmatizing language to avoid and empowering language to adopt. This is a practical toolkit for anyone who wants to be a better ally and a more compassionate communicator.
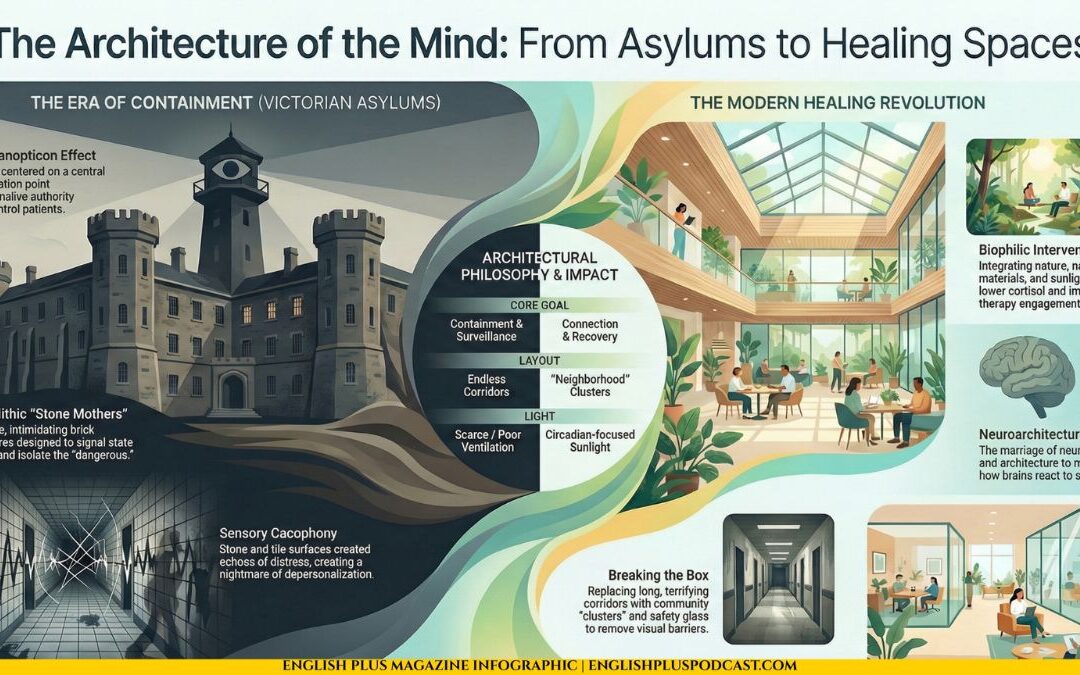
And finally, we’ll wrap up the week with A Brief History of Madness and Medicine. We’ll take a journey through time to understand how our perceptions of brain disorders have evolved, from ancient beliefs about demonic possession to the birth of the asylum, the dawn of psychoanalysis, and the modern neuroscientific revolution. Understanding our past is essential to charting a better, more humane future.
Each of these episodes is a crucial piece of a larger puzzle. By the end of this week, our hope is that you’ll not only have a richer understanding of the topic but also feel more confident and compassionate when engaging with it in your own life. This is not about shortcuts to knowledge, but about beginning a genuine, lifelong process of learning. The real work happens when you take these ideas and explore them further through your own reading, research, and conversations.
The brain is the architect of our reality. When it falters, our world can be turned upside down. But by approaching its disorders with scientific curiosity and profound human empathy, we can help turn it right side up again.
Thank you for starting this journey with me.
Let’s Discuss
And now it’s time for “Let’s Discuss.” This is the part of the show where we move from listening to engaging. The ideas we talked about today are foundational, and they often challenge long-held beliefs. Here are a few questions to get the conversation started in the comments section on our website. We’d love to hear your perspective.
- The Organ Analogy: How did the concept of the brain as just another organ that can get sick, like the heart or liver, land with you? Did it change your perspective on conditions like depression or anxiety?
- Prompts for discussion: Think about a time you or someone you know had a purely “physical” illness. Now think about an experience with a mental health challenge. Did you view them differently? Does this analogy help bridge that gap for you? Why or why not?
- Witnessing the Divide: Have you personally witnessed the societal divide in how we treat neurological conditions (like epilepsy) versus mental health conditions (like bipolar disorder)? Share your observations.
- Prompts for discussion: Consider how these conditions are portrayed in movies or TV shows. Think about conversations you’ve overheard or participated in. Where have you seen stigma in action? Conversely, have you seen positive examples that challenge this divide?
- A Unified “Brain Health”: We argued for a unified view of “brain health” instead of separating “mental” and “neurological” health. What do you see as the biggest potential benefit of this shift in perspective? Are there any potential downsides or challenges you foresee?
- Prompts for discussion: How might this change things in our healthcare system? In our schools? In our workplaces? Could it reduce stigma, or does lumping everything together risk oversimplifying complex and different experiences?
- Language and Stigma: The episode touched on how casual phrases like “I’m so OCD” can be harmful. What other examples of stigmatizing language have you noticed in everyday conversation?
- Prompts for discussion: Why do you think we resort to this kind of language? Is it just a habit, or does it reflect a deeper discomfort with the topic? What are some simple, respectful alternatives we could use instead?
- The Learning Journey: What was the single most surprising or challenging idea you heard in today’s episode? And looking at the roadmap for the week, which upcoming topic are you most curious about and why?
- Prompts for discussion: This is an invitation for self-reflection. What assumption was challenged for you today? What new question has this episode sparked in your mind? Sharing what you’re eager to learn next helps us all see what resonates most deeply.
Head over to our website, find the post for this episode, and share your thoughts. Let’s learn from each other.
Podcast Outro
And that brings us to the end of our first episode in the Mind Matters series. Thank you so much for lending me your time and your attention today as we laid this crucial groundwork.
If you want to continue this journey with us and ensure you don’t miss a single episode this week, the best way to do that is by becoming part of the English Plus ecosystem. You can find transcripts for our episodes, our entire back catalog, and the vibrant discussion section we just talked about on our website at EnglishPlusPodcast.com.
Whatever level of engagement you choose, we’re just glad to have you here. The most important thing is to keep learning, keep questioning, and keep talking.
Until tomorrow, be curious, be compassionate, and take care of that incredible organ between your ears. I’m your host, and this is English Plus.






0 Comments